Prenatal Cell Free DNA Screening 101: Toolkit for Providers
From the experts to you:
Dr. Tamar Goldwaser, MD, FACMG, FACOG is an OBGYN and a Medical Geneticist practicing in New York at Maternal Fetal Medicine Associates, where she addresses complex issues in the preconception and prenatal setting. She also is the Director of the Cancer Risk Assessment Genetics Program at Englewood Health Cancer Center in New Jersey.
SUMMARY:
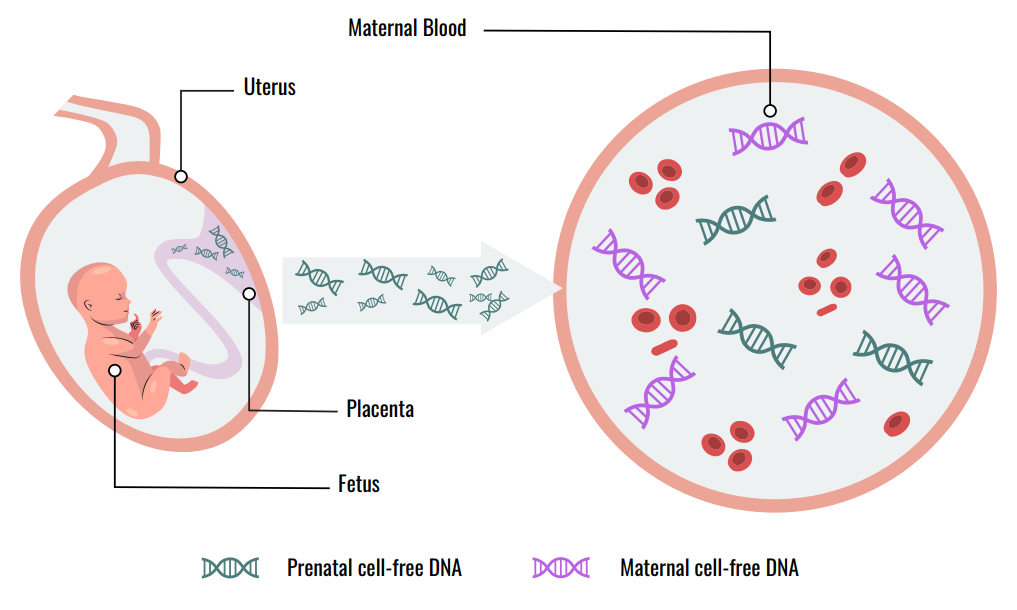
Also known as noninvasive prenatal testing (NIPT), prenatal cell-free DNA (cfDNA) based screening for fetal aneuploidy has been clinically available since 2011. cfDNA has emerged as the screening test of choice for detection of fetal common aneuploidies and sex chromosome aneuploidies (ACMG) and should be made available to all pregnant women regardless of risk (ACOG). The test is performed on a maternal blood sample and based on free-floating placental DNA fragments that are detected in the maternal serum, mixed with cell-free maternal DNA fragments. Most cfDNA technologies use next-generation sequencing followed by high level computational algorithms that generate data for patient reports. The underlying technologies and bioinformatics have advanced sufficiently such that currently, cfDNA analysis can screen for far more than just the common aneuploidies.
Prenatal Genetic Screening Basics
- All pregnancies have a risk for genetic abnormalities, regardless of maternal age
- 1 in 150 livebirths have a genetic abnormality
- Genetic disorders can include
- Chromosomal disorders including aneuploidy: Deletions or duplications of either entire chromosomes or partial segments of chromosomes that can affect multiple genes
- Single gene disorders: Changes in DNA sequence within a gene that can result in disease
- Since the early 1980s, maternal screening for fetal aneuploidy such as Down syndrome has been available as part of prenatal care
- These screening tests are a key component of prenatal care but have important limitations
- Positive screening tests always need to be confirmed
- cfDNA assesses placental DNA that does not always accurately reflect true fetal DNA
- Negative screening tests always have associated residual risks
- ACOG, SMFM and ACMG all recommend offering all pregnant women the option of invasive diagnostic testing for aneuploidy regardless of maternal age or risk
- By definition, screening tests are less accurate than diagnostic testing such as amniocentesis or chorionic villus sampling (CVS)
Current Guidelines
ACMG
- For both singleton and twin pregnancies, ACMG recommends offering cfDNA as first line fetal aneuploidy screening over standard screening (biomarkers and ultrasound) for
- Down syndrome: Trisomy 21 (T21)
- Edward syndrome: Trisomy 18 (T18)
- Patau syndrome: Trisomy 13 (T13)
- Fetal sex chromosome aneuploidies (SCA) such as Turner syndrome (45,X), Triple X syndrome (XXX), Jacobs syndrome (XYY), and Klinefelter syndrome (47,XXY)
- ACMG Suggests offering prenatal cfDNA screening for
- 22q11 deletion syndrome (DiGeorge syndrome)
- ACMG does not recommend against testing for additional CNVs and rare autosomal trisomies (i.e., not including 13, 18, 21, X and Y) but rather states “Insufficient Evidence to Recommend”
ACOG/SMFM
- cfDNA is recognized as “the most sensitive and specific screening test for the common fetal aneuploidies”
- Options include
- Aneuploidy screening with cfDNA or
- First trimester serum screening with or without nuchal translucency
- ACOG and SMFM do not recommend screening for CNVs due to concerns regarding detection and false-positive rates
PRETEST COUNSELING – KEY POINTS
Options for Aneuploidy Screening in the First Trimester
First Trimester Screening (biomarkers and first trimester ultrasound)
- Benefits
- Simple blood test performed between 11 and 14 weeks using beta-human chorionic gonadotrophin (free or total hCG) and pregnancy-associated plasma protein A (PAPP-A) represents serum portion
- First trimester ultrasound component with NT can detect structural and placental abnormalities as well as additional chromosome or single gene defects
- Relatively high detection rate for T21 | Can also detect other common aneuploidies especially T18
- Typically will return a result
- Carries no procedure-related risk
- Concerns
- Lower detection rate for common aneuploidies vs cfDNA
- PPV is approximately 5% for T21 | Only 1 in 20 women with a positive result will actually have a fetus affected with T21 and therefore many women will experience unnecessary anxiety, emotional distress and invasive testing they may not have otherwise opted for
- Does not include sex chromosome aneuploidies
- NT measurement, unlike laboratory testing, requires proximity to an advanced ultrasound unit with training and expertise and should only be performed by NT certified sonographers | Potential equity issue
- Performance less robust in twin vs singleton pregnancies
cfDNA
- Benefits
- ACMG considers cfDNA superior and the first line choice for prenatal aneuploidy screening | ACOG recommends cfDNA be offered to all women as an option for prenatal aneuploidy screening
- Performed as early as 9 weeks | Single visit | No ultrasound needed | Can do at any point in pregnancy
- cfDNA consistently outperforms standard screening especially for T21 (ACMG)
- Detection Rate: 98.8% vs 82%
- False Positive Rate: 0.04% vs 5.6%
- Positive predictive value (PPV), indicating the chance a screen positive result will be confirmed as a true positive, is substantially higher for cfDNA vs standard screening, especially for T21 regardless of maternal age
- cfDNA: 91.8%
- Traditional Screening: 3.6%
- Only screening test available that can identify
- Fetal sex and sex chromosome aneuploidies
- Microdeletion syndromes
- Genome wide changes including copy number and all aneuploidies
- Concerns
- Because the detection rate and PPV are so high, it is easy for patients to get confused and consider cfDNA a diagnostic test vs a screening test
- Unlike standard screening, a positive cfDNA often represents a true positive but it is not 100% and confirmation is still required for a definitive diagnosis
- Negative predictive value (NPV) of a chromosome abnormality following a negative result is very low but not 0%
- A ‘no call’ is possible (approximately 1%) and is more likely in patients with
- High BMI | Exposure to LMWH | Fetal aneuploidy especially T13 and T18
- Report may also return with “higher risk for maternal malignancy” due to multiple chromosomal aberration signals detected on cfDNA or may be abnormal due to maternal mosaicism
WHAT DISORDERS ARE COVERED WITH cfDNA?
Both ACMG and ACOG/SMFM Recommend
Common Aneuploidies
- T21: >99% detection rate for T21
- 98% detection rate for T18
- 99% detection rate for T13
- Combined false positive rate of 0.13%
- cfDNA is the most sensitive and specific screen for T21, T18 and T13
ACMG Also Recommends
Sex chromosome abnormalities
- Benefits
- Certain sex chromosome aneuploidies such as Turner syndrome may have higher rate of fetal malformation and warrant fetal echocardiogram
- Early treatment of Klinefelter syndrome in childhood may be advantageous
- Concerns
- Subject to false positive test results
Note: A result consistent with Turner syndrome may reflect the maternal chromosomal complement and not fetal | Any suspicion for preexisting maternal mosaic Turner syndrome should prompt referral to Maternal Fetal Medicine, Genetics and Cardiology services for further follow up
ACMG Also Suggests Offering
22q11.2 Deletion Syndrome
- Benefits
- May occur in 1 in 990 to 1 in 2148 pregnancies | Higher prevalence than T21 in pregnancies of younger women
- Cases can be missed at birth leading to diagnostic odyssey for parents
- PPV reported to be as high as 52.6% (although may be lower in a truly low risk population without any structural abnormalities)
- Negative predictive value (NPV) is >99%
- Concerns
- Similar to other disorders, positive screening result requires follow-up confirmation with definitive genetic testing
Other Chromosomal Abnormalities – CNVs
Targeted Microdeletions
- Benefits
- There are other microdeletion syndromes aside from 22q11.2 deletion syndrome that carry significant morbidity and mortality
- cfDNA offers a noninvasive approach to detect some of these microdeletions associated with significant clinical outcomes
- Conditions screened that are severe may include
- Prader Willi/Angelman Syndrome | Cri-du-chat | Wolf Hirshhorn syndrome
- Concerns
- Not recommended by ACOG/SMFM due to concerns regarding detection and false positive rates | Women who want information on microdeletions should be offered microarray from CVS or amnio specimen
- ACMG notes that “there will be families for whom cfDNA for CNVs could be offered based on the pregnancy or family history” and recommend consultation with a genetic service
- PPV is lower due to lower prevalence of disease
Genome-Wide Changes (not targeted)
- Benefits
- Analyzes chromosomal changes across the genome
- The rare autosomal aneuploidies have been associated with adverse pregnancy events though currently no way to predict precise pregnancy outcomes
- Concerns
- Incidental findings are more likely to occur with genome-wide vs more targeted cfDNA
- Crucial to counsel patients that genome-wide cfDNA may miss clinically significant findings detectable with invasive diagnostic testing using microarrays
- Generally genome-wide screening for additional CNVs and rare autosomal trisomies is not recommended by professional organizations for routine screening
POSTTEST COUNSELING – KEY POINTS
Positive Screen Result
What is the Chance the Positive Report will Be a True Positive?
- PPV is the critical performance characteristic for posttest counseling and refers to the likelihood that the patient’s positive cfDNA report actually correlates with a definitive diagnosis
- T21: PPV 91.8%
- T18: PPV 65.8%
- T13: PPV 37.2%
- Lower with T18 and T13 because of lower prevalence
- Important to counsel regarding PPV for particular aneuploidy where a report is screen positive
- PPV will change based on maternal age and a priori risk based on presence or absence of ultrasound findings
- PPV may be either found on reports or can use specific calculators
What Can Cause a False Positive?
- Less likely for T21 but can occur | More common with T18 and T13
- Biological causes include
- Mosaicism (mixture of abnormal and normal cell lines) | Confined placental mosaicism can lead to false positive result since cfDNA analyzes DNA fragments from placenta
- Vanishing twin | More likely to be aneuploid and residual abnormal cells may be retained in the placenta
- Maternal malignancy (see below)
- Maternal chromosomal abnormality
What are Next Steps Following a Positive Result?
- Recommend detailed ultrasound (including fetal echocardiogram) and genetic counseling services
- Key point: Confirm result with diagnostic testing
- CVS or amniocentesis are both considered options
- If cfDNA is positive for T13 or Turner syndrome and especially if ultrasound looks normal, strongly consider amniocentesis over CVS given higher risk of CPM
- Confirmation of microdeletions requires microarray and will be missed with standard karyotype alone | Additional molecular testing may be required based on the particular disorder that was detected on screening
- If testing declined, management based on sonographic features and patient desires
- Serial ultrasounds for care plan
- Neonatal karyotype with additional testing such as microarray and molecular testing depending on the disorder
Negative Screen Result
What is the Chance the Negative Report will Be a True Negative?
- NPV, which indicates that a negative report is truly negative, is >99%
What Can Cause a False Negative?
- Possible explanations for a false-negative test result
- Sample labeling error
- Low fetal fraction
- Possibility of a mosaicism that is present at low levels in the placenta
What are Next Steps Following a Negative Result?
- Patient can be reassured with a screen negative report, but should be aware that there is always a residual risk with any screening test
- Still may choose invasive testing especially if ultrasound findings concerning
- If congenital anomalies are found on ultrasound, cfDNA should not be considered sufficient
- Invasive testing should be offered
- Other chromosomal anomalies may be detected on microarray that are not covered by cfDNA
Next Steps Following ‘No Call’
- Insufficient fetal fraction will result in a ‘no call’
- Increased risk of aneuploidy with this finding, particularly T18, T13 and SCAs (likely due to smaller placentas)
- Repeat only if early GA may have compromised result
- Offer definitive testing and early ultrasound
Next Steps Following ‘Risk for Maternal Malignancy’
- Report may return with risk for maternal malignancy due to multiple chromosomal aberration signals detected on cfDNA
- Currently, there are no standardized professional guidelines for next steps following a cfDNA result suggesting possible maternal malignancy
- Suggested work up for malignancy includes consideration of the following
- Patient’s desire for information | Costs | Personal history | Family history
- Workup can include
- Detailed medical history | Comprehensive physical exam | Labs | Imaging
- Referral to an oncology specialist should also be considered
- If multiple or unusual aneuploidies detected not suggested of malignancy should still refer to genetics and MFM
- Physicians can refer patients to ongoing studies
- The IDENTIFY study at the NIH is an option for patients with abnormal or non-reportable noninvasive prenatal testing results (see ‘Learn More – Primary Sources’ below)
KEY POINTS:
- cfDNA utilizes next generation sequencing to look at the DNA fragments in the mother and fetus to determine the likelihood of certain genetic conditions in the fetus
- While there are multiple panels available, there is consensus regarding the clinical utility of cfDNA screening for T13, T18 and T21
- Patient education, especially around the concept of positive predictive value (PPV) is a priority
- Calculator tools are available from professional societies and laboratories’ real world test performance results
- Beyond common aneuploidies, cfDNA can also be used to screen for
- Sex chromosome aneuploidy | Copy number variants across the genome | Select microdeletions
- Counseling patients regarding these results can be nuanced
- Result of increased risk of maternal malignancy can also occur during testing with cfDNA
- Ability of provider to perform pretest and posttest counseling imperative to offering test
- First trimester NT not needed with negative cfDNA
- Second trimester ultrasound should be offered to all pregnant women independent of cfDNA to assess for structural anomalies
- All professional societies emphasize that clinical decisions should be based on results of confirmatory diagnostic testing and not on screening results, particularly termination of pregnancy
- Standard karyotyping on a CVS or amniocentesis specimen may not be sufficient for confirmation
- Microdeletion confirmation requires microarray analysis due to small size of absent sequence
- Some microdeletion syndromes may require specialized testing for uniparental disomy that can detect whether the missing sequence is maternal or paternal in origin
LEARN MORE – PRIMARY SOURCES:
ACOG Practice Bulletin 226: Screening for Fetal Chromosomal Abnormalities | ACOG
SMFM Consult Series #42, The role of ultrasound in women who undergo cell-free DNA screening
DNA sequencing versus standard prenatal aneuploidy screening (Bianchi et al., NEJM 2014)
Cell-free DNA analysis for noninvasive examination of trisomy (Norton et al., NEJM 2015)
NIPT Predictive Value Calculator (perinatalquality.org)
Commercial Support:
Support provided by Illumina
Financial Disclosures:
Dr. Goldwaser reports that she has no relevant financial relationships to disclose
